IAHN








Editor-in-Chief: Janusz Ostrowski
Deputy Editor-in-Chief: Davide Viggiano
Editors: Maria Kalientzidou, Guido Gembillo
IAHN Bulletin is the official E-Newsletter of the International Association for the History of Nephrology
Bulletin
No. 12, June 2024
www.iahn.info

Despite
the
very
difficult
and
complicated
political
situation
in
the
world,
scientific
societies,
including
our
own,
continue
to
fulfil
their
statutory
roles
without
interruption.
The
editorial
team
of
the
Bulletin
of
the
International
Society
for
the
History
of
Nephrology
proudly
presents
its
12th
issue
to
our
readers,
society
members,
and
supporters.
We
are
striving
to
make
the
Bulletin
increasingly
attractive.
This
issue
features
a
slightly
revised
graphic
design,
which
we
hope
will
be
well
received by our readers.
Among
the
authors
of
the
publications
are
our
regular
contributors,
Natale
De
Santo,
Katarina
Derzsiova,
Maria
Kalientzidou,
Guido
Gembillo,
Malcolm
Philips,
and
Andrzej
Więcek.
The
main
topics
include
works
on
two
distinguished
nephrologists
who
have
passed
away
this
year,
Zbylut
Twardowski
and
Dimitar
Nenov;
publications
related
to
the
100th
anniversary
of
the
first
human
haemodialysis;
a
report
from
the
conference
dedicated
to
Stewart
Cameron
in
London;
information
about
important
nephrology-related
events
in
Poland;
and
the
latest
news
about
the
upcoming
IAHN
congress in Naples, Italy.
Since
the
IAHN
Bulletin
is
an
e-newsletter,
we
have
even
greater
publishing
capabilities.
We
encourage
all
readers
to
submit
materials
about
notable
individuals
and
events
in
their
respective
countries,
achievements
of
IAHN
members,
and
historical articles.
We
are
all
eagerly
anticipating
the
opportunity
to
gather
with
friends
in
Naples,
which
we
hope
will
be
another
important
step in the development of our society.
I wish everyone a wonderful holiday and a good rest.
Janusz Ostrowski
Editor-in-Chief


Janusz Ostrowski
Board of the International Association for the History of Nephrology


President - Ayse Balat
PAST President - Iwannis Stefanidis
President ELECT - Davide Viggiano
TREASURER - Vincenzo Savica
EX OFFICIO - Natale De Santo
INTRODUCTION
Professor, Department of the History of Medicine,
Centre of Postgraduate Medical Education, Warsaw, Poland
janusz.ostrowski@cmkp.edu.pl
Janusz Ostrowski
One
hundred
years
ago,
in
1923,
Georg
Haas
(1886-1971)
performed
the
first
haemodialysis
on
a
human
being
in
the
German
city
of
Giessen
.
Before
him
were
John
Abel,
Leonard
Rowntree
and
B.
Turner
from
Johns
Hopkins
University
in
Baltimore
were
the
first
scientists
to
apply
the
concept
of
dialysis
to
dogs.
Haas
designed
a
dialyser
that
used
collodion
tubes with Ringer's solution as the dialysate.
As
for
anticoagulation,
he
was
also
the
first
to
consider
a
possible
role
for
citrate,
but
was
ultimately
convinced
that
hirudin was the better choice, regardless of its cost and toxicity.
The
aim
of
this
first
haemodialysis
was
merely
to
prove
its
safety,
and
therefore
the
procedure
lasted
only
fifteen
minutes.
Between
1925
and
1926,
another
5
patients
were
dialysed,
but
the
toxicity
of
hirudin
prevented
further
improvements.
In
1928,
the
newly
available
anticoagulant
heparin
enabled
Haas
to
treat
three
more
patients
with
what
was
known
as
fractionated
dialysis,
in
which
400
ml
of
blood
was
taken
from
the
patients,
heparinised
and
then
passed
through
the
dialyser
in
nine
separate
sessions.
The
German
scientist
also
noticed
the
decrease
in
blood
volume,
which
he
attributed
to
the
overpressure
in
the
blood
compartment.
He
was
also
the
first
to
consider
haemodialysis
as
a
possible
treatment
for
nephrotic oedema.
When
he
presented
his
work
at
a
medical
congress
in
Wiesbaden
in
1927
,
he
was
severely
criticised
and
abandoned
his
work.
Looking
back
on
his
journey,
he
said:
"From
the
first
idea
to
the
actual
realisation
of
the
dialysis
method
was
a
very
long
way.
I
would
say
it
was
a
via
dolorosa!".
Despite
all
the
difficulties,
his
experiments
contributed
significantly
to
a
better knowledge of haemodialysis and represented a milestone in the field of nephrology.
References:
1
Haas G. Dialysis of the flowing blood in the patient. Klin Wochenschr 1923: 70, 1888.
2
Haas G. Die Methoden der Blutauswaschung. Aberhandeln’s hanb Biol Arbeitsmethoden V 1935 (8): 717-754
Janusz Ostrowski


A CENTURY AFTER THE FIRST HUMAN HAEMODIALYSIS,
A MILESTONE IN NEPHROLOGY.
1
University of Messina, Unit of Nephrology and Dialysis, Department of Clinical and
Experimental Medicine, Messina, Italy.
2
Italy University of Messina, Department of Biomedical, Dental, Morphological and
Functional Imaging Sciences, Messina, Italy.
3
A. Monroy Institute of Biomedicine and Molecular Immunology, National
Research Council, Palermo.
Guido Gembillo
1,2
; Guido Bellinghieri
1
; Luigi Peritore
1
;
Vincenzo Savica
2
and Domenico Santoro
1

Introduction
Once
upon
a
time,
a
young
doctor
was
prescribing
in
despair
the
“death
recipe”
for
his
patient
dying
from
uremia.
All
that
he could offer was early euthanasia.
“…Paraldehyde
gives
a
very
natural
and
dreamless
sleep.
The
dose
can
be
repeated
whenever
the
patient
shows
signs
of
restlessness
and
the
quantity
given
can
be
safely
increased
up
to
as
much
as
60cc
every
6hr
or
so,
for
here
also
uremia
seems
to
carry
with
it
a
greatly
increased
tolerance,
and
there
is
a
wide
margin
between
the
dose
that
makes
the
patient
just
drowsily
unconscious
and
the
amount
required
to
induce
a
deep
sleep.
It
is
the
quiet
drowsiness
we
want.
The
disease itself will soon bring the deep sleep. [1] “
Once upon a time, a young doctor was shocked by the sudden death of his favourite 26 years old actress Jean Harlow
“On
June
6,
1937,
Harlow
said
that
she
could
not
see
Powell
clearly
and
could
not
tell
how
many
fingers
he
was
holding
up.
That
evening,
she
was
taken
to
Good
Samaritan
Hospital
in
Los
Angeles,
where
she
slipped
into
a
coma.
The
next
day
at
11:37
a.m.,
Harlow
died
in
the
hospital
at
the
age
of
26.
In
the
doctor's
press
releases,
the
cause
of
death
was
given
as
cerebral oedema, a complication of kidney failure. Hospital records mention uremia…[2]…”
Once
upon
a
time
back
in
the
19th
century,
a
Scottish
chemist
Thomas
Graham
was
studying
in
his
chemical
laboratory
and
publishing
his
work
about
the
methods
of
osmosis
and
dialysis
used
for
the
separation
of
dissolved
substances
or
the
removal
of
water
from
solutions
through
semipermeable
membranes.
He
introduced
the
concept
of
diffusion
across
a
semipermeable membrane, termed it “dialysis” in 1861[3,4].
Once
upon
a
time,
three
scientists
(Abel
JJ,
Rowntree
LG,
Turner
BB)
applied
the
principle
of
diffusion
to
the
removal
of
substances
from
the
blood
of
anaesthetized
animals.
They
dialyzed
them
by
directing
their
blood
outside
their
body
and
through
tubes
of
semipermeable
membranes
made
from
a
material
based
on
cellulose[5].
In
two
papers
published
in
1914,
they
gave
a
much
more
detailed
account
of
their
apparatus
which
they
called
an
artificial
kidney[6,7].
They
tried
to
inhibit
blood
clotting
or
coagulation
by
using
a
substance
known
as
hirudin,
which
had
been
identified
as
the
anticoagulant
element
in
the
saliva
of
leeches
in
1880.
The
very
high
price
of
hirudin,
USS
27.50/g
in
1914,
just
enough
for
two
experiments,
forced
them
to
prepare
their
own
leech
extracts,
but
they
were
very
toxic,
so
they
abandoned
this
field
of investigation and the potential use of the artificial kidney in humans. Heparin had not yet been discovered.
Once
upon
a
time,
a
German
doctor
(Georg
Haas)
started
performing
preparatory
experiments
on
dialysis
treatments
involving
humans.
It
is
believed
that
he
dialyzed
the
first
patient
with
kidney
failure
in
the
summer
of
1924
and
this
first
human
dialysis
lasted
only
15
min.
By
1928
he
had
dialyzed
six
patients,
none
of
whom
survived,
likely
because
of
the
critical condition of the patients and the ineffectiveness of the dialysis treatment[8,9]. He stated :
“….
I
know
that
one
swallow
still
doesn’t
make
a
summer-
but
despite
the
limited
number
of
observations,
I
have
already
gotten
the
distinct
impression
that
is
worth
the
effort
to
continue
along
the
path
taken.”
He
also
used
hirudin
as
the
anticoagulant in his dialysis treatments.
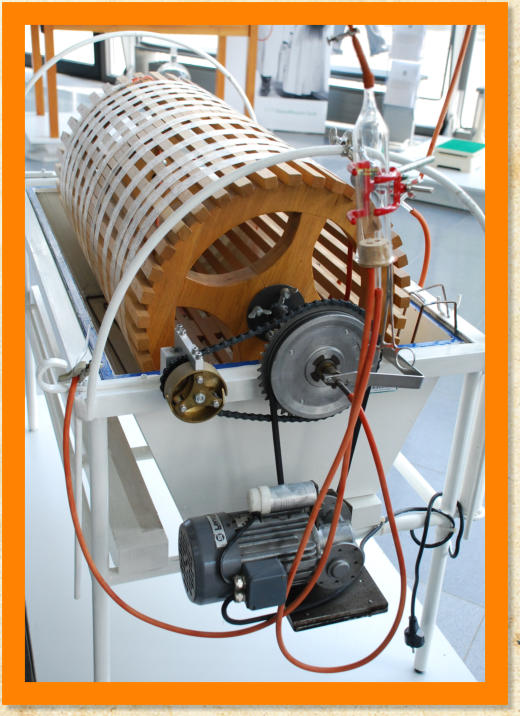
Once
upon
a
time,
in
the
fall
of
1945
science
credited
a
doctor
from
the
Netherlands,
Willem
Kolf,
with
the
first
successful
dialysis
in
humans.
He
used
a
rotating
drum
kidney
with
membranous
tubes
made
from
a
new
cellulose-
based
material
known
as
cellophane.
The
blood-filled
tubes
were
wrapped
around
the
wooden
drum
that
rotated
through
an
electrolyte
solution,
the
dialysate,
causing
the
uremic
toxins
to
pass
into
this
rinsing
liquid[10,11].
Heparin
already adopted by Hass in 1937, replaced the toxic and expensive hirudin.
Once upon a time dialysis was not indicated for treatment of chronic renal failure. Kolf stated in 1946:
“Chronic
nephritis
is
no
indication
for
treatment
with
the
artificial
kidney,
though
an
acute
exacerbation
of
chronic
uremia
might
be
an
indication
in
some
cases.
An
acute
uremia,
whatever
the
cause
may
be,
is
an
indication
for
treatment
with the artificial kidney as soon as it immediately threatens the patient’s life…..” [12].
Once
upon
a
time,
a
tale
of
continuous
improvements
and
technological
advancements
began
concerning
the
effectiveness of dialyzers, methods of dialysis, machine modification, and vascular access.
Once
upon
a
time,
the
expectation
of
long-term
treatment
of
patients
with
chronic
kidney
failure
became
true.
In
1960
Scribner
implanted
a
shunt
in
an
American
patient[13].
This
success
provided
the
basis
for
the
chronic
hemodialysis
sessions.
Once
upon
a
time
(in
the
early
1970s)
dialysis
treatments
lasted
around
12
hours
and
were
very
expensive.
Consequently,
not
all
patients
had
access,
choices
about
who
would
receive
dialysis
were
made
by
an
anonymous
committee,
the
first
bioethics
committee.
External
shunts
were
followed
in
1967
by
the
work
of
Brescia
and
Cimino[14]
which
was
followed
by
the development of synthetic grafts and central vein double-lumen catheters in the 1980s.
Once
upon
a
time
a
breakthrough
of
developments
started
concerning
dialysis
facilities,
technical
advances,
dialysis
machines
with
proportioning
pumps,
improved
monitoring
devices,
bicarbonate
dialysis,
drugs
(new
antihypertensive,
vitamin D derivatives, parenteral iron compounds, erythropoietin) long nocturnal or short daily dialysis.
Dialysis: a life-prolonging or a life-saving process but not a life-«salving» process
Dilemmas
concerning
the
life-prolonging
or
life-saving
character
of
dialysis
treatment
are
prominent,
especially
in
the
elderly
and
how
to
identify
and
deal
with
the
concept
that
dialysis
treatment
seems
to
prolong
suffering
and
the
process
of
dying
rather
than
adding
quality
days
to
the
patient's
life.
A
crucial
“trilemma”
then
arises:
whether
dialysis
treatment
can
be
considered
life-saving,
life-prolonging
or
life-«salving»
since
dialysis-treated
patients
may
often
continue
to
experience
feelings
of
anxiety,
insecurity,
frustration
escorted
by
guilt
over
the
burden
on
the
family
and
poor
quality
of
life under hemodialysis treatment.
It
is
well
known
that
hemodialysis,
particularly
intermittent,
is
a
non-physiologic,
physio-chemical
treatment
and
is
unable
to
restore
the
constancy
of
the
internal
environment
achieved
by
the
kidney.
Raghavan
and
Eknoyan
pointed
out:
“Suffice
it
to
say
that
dialysis
is
an
empiric
treatment.
There
are
no
clinical
trials
or
experimental
studies
of
the
long-term
effects
of
dialysis
on
normal
bodily
functions,
either
in
the
presence
of
normal
or
reduced
kidney
function.
Similarly,
there
are
no
studies
of
the
long-term
cardiovascular
effects
of
arteriovenous
fistulas,
no
matter
how
modest
their
continued
blood
flow
may
be.
Dialysis
operates
on
principles
that
are
the
very
opposite
of
what
homeostasis
is
all
about.
Where
homeostasis
is
fine-tuned
to
adjust
and
maintain
the
normalcy
of
any
abnormal
change
in
the
composition
of
the
bodily
fluids
to
a
mean
or
median
within
a
rather
narrow
range
of
“normal”,
dialysis
provides
no
such
fine
adjustment
or
maintenance……”[15].
These
comments
do
not
underestimate
the
life-saving
effect
that
dialysis
provides.
According
to
the
authors’
concept
for
any
given
patient
the
moral
difference
between
prolonging
dying,
life-prolonging
and
life-saving
may
be
“artificial”,
especially
in
the
case
of
dialysis
where
the
prolonging/saving
life
(which
is
always
of
the
first
importance
of
a
treatment)
of
the
patient
extends
to
many
years
in
the
majority
of
patients.
Hence
if
all
our
days
are
of
equal
worth,
it
would
seem
to
follow
that
the
dying
days
of
a
patient
would
need
to
be
prolonged
no
less
vigorously
than
any
other
days.
To
speak
of
a
treatment
which
prolongs
dying
is
probably
a
misleading
way
to
speak
of
treatment
which
prolongs
life
provided
that
we
can
distinguish
between
those
patients
who
are
dying
and
those
who
are
not.
The
term
dialysis
comes
from
the
Greek
word
which
in
the
Greek
language
has
a
double
meaning:
firstly
the
scientific
one
refers
to
the
separation
of
crystalloids
from
colloids
in
a
solution
by
diffusion
through
a
membrane
and
secondly,
the
rational
one
refers
to
adverse
happenings
suddenly
occurring,
causing
great
damage.
In
the
case
of
end-stage
renal
patients,
the
first
one
applies
to
the
hemodialysis
process
and
treatment
of
the
renal
patient
the
second,
sometimes
more
prominent,
to
the
life
of
end
end-
stage
renal
disease
patient.
In
the
future,
there
are
expectations
concerning
novel
more
challenging
and
promising
approaches (artificial intelligence, stem cells, kidney organoids) that improve the quality of life of renal patients.
Conclusion
Once
upon
a
time,
they
did
not
live
happily
ever
after.
This
nephrology
tale
has
no
end.
On
the
contrary,
scientists
continue
to
be
challenged,
to
hope,
to
be
in
despair,
to
be
shocked,
to
study,
to
apply,
to
try
to
inhibit,
to
abandon,
to
perform
experiments,
to
continue
along
the
taken
path
and
always
working
for
the
beneficence
of
human
suffering
and
disease.
I
always
remember
the
words
of
a
patient
of
mine
who
was
on
dialysis
treatment
for
15
years
and
died
48
years
old:
“During
the
first
half
of
my
treatment
I
was
fighting
to
live
and
the
second
half
to
die”.
Α
struggle
in
which
desperation
and serenity and resignation and routine and fatigue and silence coexist.
In
conclusion,
after
the
initial
100-year-old
revolutionary
concept
of
dialysis
treatment,
a
question
and
a
“demanding”
wish
to
hover
over
the
need
for
the
urgent
emergence
of
an
equally
innovative
concept
that
will
be
the
“salving”
treatment
for
patients with end-stage chronic kidney disease.
References
1.
Addis T: Glomerulonephritis diagnosis and treatment. New York: Macmillan Company 1949.
2.
Pitkin,
Roy:
Whom
the
Gods
Love
Die
Young:
A
Modern
Medical
Perspective
on
Illnesses
that
Caused
the
Early
Death
of Famous People.RoseDog Books December 10, 2008. Dorrance Publishing. ISBN 978-1-4349-9199-7.
3.
Graham T: The Bakerian Lecture on Osmotic Force. Phil Trans R Soc Lond 1854; 177-228.
4.
Graham T: Liquid diffusion applied to the analysis.Phil Trans R Soc Lond 1861; 183-224.
5.
Abel
JJ,
Rowntree
LG,
Turner
BB:
On
the
removal
of
diffusable
substances
from
the
circulating
blood
by
means
of
dialysis. Transactions of the Association of American Physicians, 1913. Transfus Sci. 1990; 11(2):164-5. PMID: 10160880.
6.
Abel
JJ,
Rowntree
LG,
Turner
BB:
On
the
removal
of
diffusable
substances
from
the
circulating
blood
of
living
animals
by dialysis. J Pharmacol Exp Ther 1914; 5:275-316.
7.
Abel
JJ,
Rowntree
LG,
Turner
BB:
On
the
removal
of
diffusable
substances
from
the
circulating
blood
of
living
animals
by dialysis II: Some constituents of the blood J Pharmacol Exp Ther 1914; 5:611-623.
8.
Haas G: Versuch der Blutauswaschung am Lebenden mit Hilfe der Dialyse, Klin Wochenschr 1925; 4:13-14.
9.
Haas G: Uber Blutauswaschung. Klin Wochenschr 1928; 7:1356-1362.
10.
Kolff
WJ,
Berk
HTJ,
ter
Welle
M,
van
der
Ley
AJW,
van
Dijk
EC,
van
Noordwijk
J:
The
artificial
kidney:
A
dialyzer
with
great area. Acta Med Scand 1944; 117:121-134.
11.
Kolff WJ: The Artificial Kidney. Kampen, Kok, 1946.
12.
Gottschalk
CW,
Fellner
SK.
History
of
the
science
of
dialysis.
Am
J
Nephrol.
1997;
17(3-4):289-98.
doi:
10.1159/000169116.
PMID: 9189249.
13.
Scribner
BH,
Buri
R,
Caner
JE,
Hegstrom
R,
Burnell
JM.
The
treatment
of
chronic
uremia
by
means
of
intermittent
hemodialysis: a preliminary report. Trans Am Soc Artif Intern Organs. 1960 Apr 10-11;6:114-22. PMID: 13749429.
14.
Brescia
MJ,
Cimino
JE,
Appel
K,
Hurwich
BJ.
Chronic
hemodialysis
using
venipuncture
and
a
surgically
created
arteriovenous fistula. N Engl J Med. 1966 Nov 17; 275(20): 1089-92. doi: 10.1056/NEJM196611172752002. PMID: 5923023.
15.
Raghavan
R,
Eknoyan
G.
Uremia:
A
historical
reappraisal
of
what
happened
.
Clin
Nephrol.
2018
May;
89(5):
305-313.
doi:
10.5414/CN109401. PMID: 29451473.
Janusz Ostrowski


ONCE UPON A TIME: A FAIRY TALE FOR THE 100 YEARS
SINCE THE FIRST CONCEPT OF HEMODIALYSIS
Renal Unit/Nephrology Department, General Hospital of Kavala,
Greece
Maria Kalientzidou

Janusz Ostrowski


DIMITAR NENOV (1933 - 2024), THE DOYEN OF BULGARIAN NEPHROLOGY,
DISTINGUISHED PROFESSOR AT THE UNIVERSITY OF VARNA BEHIND THE
IRON CURTAIN AND PRESIDENT OF BULGARIAN BRANCH OF PROFESSORS
EMERITI
1
University Luigi Vanvitelli Naples,
2
Division of Nephrology University of Messina,
3
Scientific Director
of Biogem, Ariano Irpino (AV),
4
Division of Nephrology Annunziata Hospital Cosenza,
5
Migration Center University of Calabria at Rende,
6
Division of Nephrology Cassino Hospital,
7
Founder of Ph.D. Course in Ecology at the University Federico II, Naples,
8
Nephrological Laboratory, University hospital of Louis Pasteur,
9
Louros Foundation,
Athens,
10
Division of Nephrology University of Sarajevo,
11
Consultant in General Internal
Medicine, East Surrey Hospital, Redhill, London
Natale G. De Santo
1
, Guido Bellinghieri
2
, Giovanbattista Capasso
3
,
Nicola De Napoli
4
, Vincenzo Savica
2
, Teresa Papalia
4
,
Pantaleone Sergi
5
, Luigi Iorio
6
, Amalia Virzo
7
, Katarina Derzsiova
8
,
Halima Resic
9
, Athanasios Diamandopoulos
10
, Veselin Nenov
11

Early Life and Studies
Dimitar
Nenov(Figure
1),
was
born
on
May
2,
1933
in
the
village
of
Pobit
Kamak,
district
of
Razgradin
in
Bulgaria.
He
had
just
completed
primary
school,
when,
due
to
the
Socialistic
Revolution
of
September
9,
1944,
Bulgaria
entered
in
the
orbit
of
USRR
and
collectivism
became
the
new
state
model
and
his
family
property
were
confiscated.
He
completed
Junior
high
school
in
Pobit
Kamak
and
the
high
school
in
in the town of Russe.
He
registered
at
the
Medical
High
School
of
Sophia
and
was
a
brilliant
student.
He
obtained
the
MD
in
1957.
Before
completing
the
medical
studies
he
got
married
with
Liliana,
a
future
Professor
of
Modern
Languages.
Physician
in
the
District
Hospital
of
Burgas.
Trainining
in Internal Medicine and Nephrology
Dimitar
moved
to
the
District
Hospital
of
Burgas,
the
hometown
of
his
wife.
In
1962
he
specialized
in
Intenal
medicìne
and
moved
to
the
Chair
of
Medical
therapy
in
the
newly
founded
Medical
School
of
Varna.
He
was
appointed
assistant
(1962)
and
later
senior
teaching
assistant
(1966). He decided to specialize in Nephrology, a branch of medicine in
great
expansion
that
had
been
recently
recognized
worldwide.
He
looked
for
an
international
training
that
at
that
time
was
available
in
a
few
places
due
to
the
vision
of
a
few
internists
who
wanted
to
explore
the
possibilities
offered
by
technology
and
organ
transplantation
(the
kidney
was
the
first
organ
successfully
transplanted).
He
could
join
the
training
programs
in
nephrology
of
the
Universities
of
Prague
(Professor
Jan
Brod),
and
in
later
years
Bologna
(Prof.
Vittorio
Bonomini),
Parma
and
Moscow.
In
Prague
he
worked
at
the
Institute
of
Cardiovascular
Research,
a
WHO
Center
for
training
on
Cardiovascular
and
Kidney
disease.
Brod,
a
libertarian
who
had
fought
nazism
and
contributed
to
liberate
Italy
from
fascism
and
participated
in
the
bloody
Battle
of
Montecassino
(17
January-18
May
1944),
reinforced
Dimitar’s
love
for
freedom.
Academic career
The
whole
academic
career
of
Dimitar
Nenov
took
place
at
the
University
of
Varna.
He
obtained
Ph.D.
in
Nephrology
in
1969
and
a
Doctorate
in
Medicine
(DM)
in
1975.
He
became
associate
professor
in
Medicine
and
Director
of
the
Nephrology
Clinic
in
1973,
and
of
Full
Professor
of
Medicine
in
1985.
He
was
Chief
of
the
United
Department
of
Internal
Medicine
(1987-
1992)
and
from
1988
till
retirement
he
was
Chief
of
the
Division
of
Nephrology
and
Hematology.
He
organized
nephrology
with
international
standards
(Clinical
Nephrology,
biopsy,
hemodialysis,
peritoneal
dialysis,
plasmapheresis,
LDL
Apheresis)
and attracted to nephrology a huge group of young investigators. He also served two 4-yar terms as Vice Rector.
In
1979,
a
time
when
the
exchange
between
Bulgaria
and
Westerns
was
difficult
he
organized
in
Varna
the
4th
Danube
Symposium
in
Nephrology
.
The
event
was
held
at
a
time
when
Bulgaria
was
under
socialism
and
scientific
exchanges
between
Eastern
and
Western
Europe
was
very
limited.
A
great
number
European
scientist
participated.
In
1986
he
organized the
3rd National Conference in Nephrology
with the participation of 70 nephrologists from abroad.
In
1989,
at
a
time
the
Berlin
Wall
was
still
in
place,
he
was
one
of
the
organizers
of
the
6th
European
Colloquium
on
Renal
Physiology
in
Varna
that
took
place
at
the
Press
House:
A
cultural
event
relevant
for
the
University
and
the
City.
In
1991
Dimitar
Nenov
gave
birth
to
the
Varna
Kidney
Foundation
and
from
this
Foundation
he
established
an
Annual
International
Conference
named
“Hot
topics
in
nephrology”
and
the
journal
Aktualna
Nefrologia
.
He
became
a
co-founder
of
the
International
Federation
of
Kidney
Foundations
(IFKF).
At
that
time
he
also
established
and
tightened
the
long-
term partnership with Italian colleagues from Naples, Cosenza and Messina (Table 1.)
Table 1 - Collaborations in Italy.


Figure 2
Figure 3
Figure 1
“The
idea
of
the
founders
was
that
such
Society
would
have
a
clear
impact
on
several
aspects
of
practice
and
research
in
nephrology
and
artificial
organs
in
the
Balkans.
In
addition,
it
would
be
a
very
positive
symbolic
act
showing
that
collaborative
work
for
the
betterment
of
life
is
possible
and
desirable
in
our
area
and
that
coming
together
will
bear
better
fruits
at
the
human
and
cultural
levels…
It
will
also
send
a
very
clear
signal
to
the
outside
world
that
the
Balkans
can be a place of collaboration and mutual understanding despite the turbulent times in the Balkan Peninsula” (1).
The
First
BANTAO
Congress
was
held
in
Varna
on
September
22-24,
1995,
an
impressive
event
under
the
chairmanship
of
Dimitar
Nenov.
Professor
F.
Valderràbano,
delegate
of
the
European
Renal
Association
published
a
congress
report:
“Nephrologists of the Balkan countries meet across political frontiers and war fronts - an example to politicians! (2).”
“BANTAO:
a
new
European
medical
association
overcomes
political
obstacles.
This
is
an
extraordinary
initiative
of
nephrologists
working
in
cities
throughout
the
Balkan
countries
who
have
been
able
to
create
a
scientific
association
and
to
organize
its
first
congress,
despite
the
boundaries
of
war,
the
rupture
of
international
relations
and
other
serious
political problems which emerged in the Balkan countries after the disappearance of the former Republic of Yugoslavia”.
The BANTAO Journal
Another
milestone
in
the
life
of
BANTAO
was
the
appearance
of
the
BANTAO
Journal
(Figure
4)
in
2003,
on
occasion
of
the
VI
Congress
that
Dimitar
Nenov
organized
again
in
Varna
(3).
Professor
Momir
Polenakovic
years
later
reporting
on
that
event
wrote:
“The
historical
editors
of
the
journal
were:
2003–2005
(Dimitar
Nenov);
2005–2009
(Ali
Basci);
2009–2015
(Goce
Spasovski).
The
BANTAO
Journal
is
now
registered
on
EBSCO,
DOAJ,
SCOPUS,
and
has
become
a
strong
'glue'
among
nephrologists
from
the
Balkan
cities.
The
BANTAO
congresses
and
the
BANTAO
Journal
have
succeeded
in
elevating
nephrology
knowledge
and
thus
increased
the
standards
of
nephrology
patient
care
throughout
the
Balkans.
Standing
above
the
divisive
forces
of
politics,
language
and
war,
BANTAO
gives
a
living
example
that
collaboration
and
humility
are
feasible in times of maddening destruction” (4).

Figure 4
Figure 5
The Bulgarian Association of Professors Emeriti
Dimitar
Nenov
founded
with
10
other
Colleagues
the
Varna
Emeriti
Association
of
Professors
Emeriti
in
Varna.
Three
of
them
were
registered
in
EAPE,
and
one
of
them
came
as
delegate
to
the
Athens
International
Congress.
It
was
the
last
collaboration he had with Naples.
Epilogue
Dimitar
spoke
Russian,
French,
English,
Czech
Serbian.
A
handsome
man,
with
a
musical
voice
used
to
whisper
arias
from
operas.
After
retirement
he
was
appointed
Expert
of
the
National
Health
System
and
consultant
of
local
hospital.
He
also
started
a
private
dialysis
unit
in
Varna
and
directed
it
till
2022.
A
brain
tumour
caused
his
death
on
February
2,
2024
in
Varna,
the
City
he
had
loved,
the
city
of
the
medical
university
he
had
served
working
hard
with
his
contagious
enthusiasm, the city where his children were born and his wife still lives.
References
1.
Polenakovic
M
and
Spasovski
G.
Ideas
abd
spirit
of
the
Balkan
Cities
Association
of
Nephrology,
Dialysis,
Transplantation
and
Aartificial
Organs
(BANTAO)
connect
nephrologists
from
the
Balkan
cities-
From
the
fpundation
to
the 15th BANTAO Congress.. Macedonian Academy of Science and Arts, Sec. of Med. Sci. 2019; XL (3): 1-25.
2.
Valderrábano
F.
Nephrologists
of
the
Balkan
countries
meet
across
political
frontiers
and
war
fronts--an
example
to
politicians!
BANTAO:
a
new
European
medical
association
overcomes
political
obstacles.
Balkan
Cities
Association
of
Nephrology,
Dialysis,
Transplantation
and
Artificial
Organs.
Nephrol
Dial
Transplant.
1996
Apr;11(4):740.
doi:
10.1093/oxfordjournals.ndt.a027379. PMID: 8671877.
3.
Nenov D. BANTAO Journal, Journal of the Balkan Cities Association of Nephrology, Dialysis,
Transplantation and Artificial Organs, Varna, Kidney Foundation. BANTAOJ. 2003; 1(1):1-3 [Google Scholar].
4.
Polenakovic
M
and
Spasovski
G
The
20th
anniversary
of
BANTAO
(Balkan
Cities
Association
of
Nephrology,
Dialysis,
Transplantation and Artificial Organs) Clinical Kidney Journal,2014; 7 (2): 224–226.
5.
De
Santo
NG,
De
Santo
RM,
Perna
AF,
Anastasio
P,
Bilancio
G,
Pollastro
RM,
Di
Leo
VA,
Cirillo
M.
To
survive
is
not
enough.
Quality
of
life
in
CKD--the
need
for
a
new
generation
of
health-oriented
economists.J
Nephrol.
2008
Mar-Apr;
21
Suppl 13:S32-50.PMID: 18446731
6.
.De
Santo
N.G.,
De
Santo
R.M.,Bilancio
G,.Perna
A
M.,
Cirillo
M.
Survival
is
not
enough.
Actualna
Nefrologia
(Varna)
.
2009; 9 (in Cyrillic): 2-9
Survival is not Enough.
In
2007
the
Italian
Institute
for
>Philosophical
Sties
launched
an
initiative
names
Survival
is
not
Enough
to
support
the
needs
of
patients
with
chronic
kidney
disease
throughout
Europe,
with
the
same
format
around
the
World
Kidney
Day.
The
annual
meeting
in
the
years
2007-2020
took
place
in
more
than
70
cities
in
Europe
in
Northern
Africa
(5).
Everywhere
the
same
topic
and
format,
inviting
to
debate
:
patients
on
dialysis
or
transplanted,
living
kidney
donors,
family
members
of
deceased
organ
donors,
nurses,
technicians,
economists,
health
administrators,
jurists,
magistrates,
psychologists,
philosophers
bioethicists,
pediatricians,
nephrologist,
neurologists,
psychiatrists,
transplant
surgeons,
journalists,
medical
editors
renal
patients
and
their
associations.
In
13
years
the
event
took
place
in
some
80
cities
including
repeatedly
Naples,
Tunis,
Milan,
Koper,
Bari,
Messina,
Athens,
Gdansk,
Cairo,
Kosice,
Trieste,
Rome,
Istanbul,
Tokyo,
Gaziantep,
Nagoya,
Bucharest,
Portaria,
Adana
and
Varna
(5,6).
The
idea
was
to
put
the
patients
in
the
center
of
the
health
systems
worldwide.
“Put
the
patients
at
the
centre
of
things.
Let
the
System
again
fit
the
patient,
stop
the
tradition
of
the
patients
fitting
the
System.
Stop
thinking
that
resources
are
limited
and
demands
exceed
supply,
and
both
are
unpredictable.
Think
that
demand
is
finite
and
predictable,
supply
is
flexible
and
manageable.
Clinicians
should
stand
in
patients’
shoes
and
seeing
things
through
their
eyes”
.
(Fiona
Godlee,
Editor
BMJ
2009;
338.b588,
Feb
12).
Varna
was
one
of
the
most
active
centres
and
collaborated
to
various
publications
of
the
Italian
Institute
for
Philosophical
Studies (Figure 5).
Fig 1. 6
th
-11
th
BANTAO CONGRESS in Varma, Ohrid, Belgrade, Antalya, Sani Chalkidiki, Timisoara

6
th
BANTAO CONGRESS in Varma, 2003

6
th
BANTAO CONGRESS in Varma, 2003

7
th
BANTAO CONGRESS in Orhid, 2005
7
th
BANTAO CONGRESS in Orhid, 2005
8
th
BANTAO CONGRESS in Belgrade, 2007
8
th
BANTAO CONGRESS in Belgrade, 2007
9
th
BANTAO CONGRESS in Rixos Suntage Hotel (Belek),
Antalya, 2009
9
th
BANTAO CONGRESS in Rixos Suntage Hotel (Belek),
Antalya, 2009
10
th
BANTAO CONGRESS in Sani Beach Hotel, Sani,
Chalkidiki, Greece, 2011
10
th
BANTAO CONGRESS in Sani Beach Hotel, Sani,
Chalkidiki, Greece, 2011

11
th
BANTAO CONGRESS in Timisoara Hotel,
Romania, 2013
11
th
BANTAO CONGRESS in Timisoara Hotel,
Romania, 2013
Fig 2. 8
th
BANTAO Congress in BELGRADE

Crown Prince Alexander of Serbia
and professors Dimitar Nenov and Miroslav Mydlík

Participants at the 8
th
BANTAO Congress
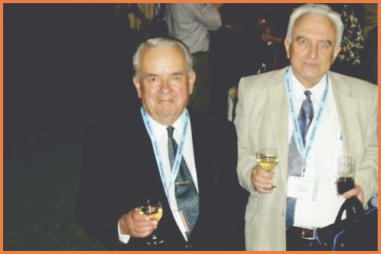
Miroslav Mydlík and Dimitar Nenov
Fig 3. Awarding the „Doctor Honoris Causa“ of P.J. Šafárik University to Professor Bonomini and 7th International
Nephrological Symposium in Košice, October 5,2006
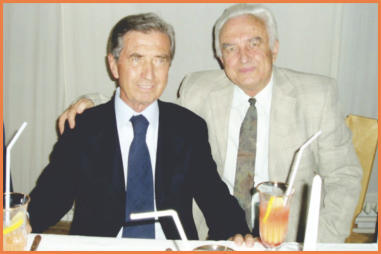
Vittorio Bonomini and Dimitar Nenov

Vittorio Bonimini and participants at Dr.H.c.

From the left: Outstanding professors: F. Kokot, G. Bellinghieri,
V. Savica, D. Nenov, M. Mydlík, V. Bonomini, W. Sulowicz

Dimitar Nenov, Guido Bellinghieri, Władysław Sulowicz

Sightseeing Tour in the Historical Part of Košice

Professor D. Nenov visiting „Nephron“,
the private Dialysis Center in Košice
Fig 4. Farewell to Dimitar Nenov

Dimitar Nenov
References
1.
Remembering Prof. Dr. Dimitar Nenov: A Tribute to the Doyen of Nephrology. February 5, 2024 by world today news.
2.
Polenakovic
M
and
Spasovski
G.
The
20th
anniversary
of
BANTAO
(Balkan
Cities
Association
of
Nephrology,
Dialysis,
Transplantation and Artificial Organs). Clin Kidney J 2014; 7: 224–226.
3.
Polenakovic
M
,
Nenov
D,
Basci
A,
et
al.
20
years
since
the
establishment
of
the
BANTAO
association
(Balkan
Cities
Association
of
Nephrology,
Dialysis,
Transplantation
and
Artificial
Organs).
Pril
(Makedon
Akad
Nauk
Umet
Odd
Med
Nauki). 2013;34(2):181-213.
4.
Mydlík
M,
Derzsiová
K,
Farkaš
M
et
al.
Renal
Tubulo-interstitial
Impairment
in
Acute
Intermittent
Porphyria
and
Variegate Porphyria. BANTAO J 2003; 1(2): 198-200.
5.
Mydlík
M,
Štubňa
J,
Tóth
Š,
Derzsiová
K,
Molčányiová
A.
Continuous
Ambulatory
Peritoneal
Dialysis
and
Pulmonary
Functions, BANTAO J 2003; 1(2): 195-197.
6.
Derzsiová
K,
Mydlík
M,
Petríková
V,
Molčányiová
A.
Haemoperfusion
of
Amitriptyline
and
Nortriptyline
–
an
in
Vitro
Study. BANTAO J 2006; 4(2): 1-4.
7.
Mydlík M, Derzsiová K. Nephrologist and Intensive Care Unit. BANTAO J 2006; 4(2): 21-24.
8.
Mydlík M, Derzsiová K. Liver and kidney damage in acute poisoning. BANTAO J 2006; 4(1): 30-33.
9.
Mydlík
M,
Derzsiová
K.
Metabolic
disorders
of
vitamin
B6
in
chronic
kidney
disease
patients.
BANTAO
J
2009;
7(2):
33-
36 .
10.
Mydlík
M,
Derzsiová
K,
Šebeková
K,
Farkaš
M,
Hvozdovičová
B,
Chmelárová
A.
Advanced
glycation
end-products
(AGEs) and long-distance run. BANTAO J 2011; 9: 67-71.
11.
Mydlik M, Derzsiova K, Čislak I. Chronic Glomerulonephritis and Pregnancy
BANTAO J 2008; 6(1): 24–26.
12.
Nenov Dimitar. Bull Eur Assoc Profs Emer 2020; 1(S1): 150-151.
An
Account
of
the
Celebration
Day
held
in
Honour
of
Stewart’s
Life
and
Work.“Stewart
Cameron. A Very Great Nephrologist”
This
celebration,
held
at
Guy’s
Hospital
on
19th
April
2024
was
attended
by
about
100
people,
including
members
of
Stewart’s family. It was recorded throughout and is available on “YouTube”.
Stewart
trained
at
Guy’s
(1953-1959)
and
was
appointed
Professor
of
Renal
Medicine
in
1974.
He
“retired”
in
1995
becoming
Emeritus Professor. He died on 30th July 2023.
The Celebration Day
The
day
was
introduced
and
co-chaired
by
Ian
Abbs,
Nephrologist
at
Guy’s
and
now
Chief
Executive
of
Guy’s
and
St
Thomas’s
NHS
Trust.
The
organiser
and
co-chairman
was
Professor
John
Feehally,
Emeritus
Professor
of
Renal
Medicine,
University of Leicester. Proceedings were in 4 sessions with 15 presenters.
In
this
account
I
have
used
names
without
titles
or
affiliations
as
in
the
Programme
of
the
Day
and
for
brevity.
(Fig
2
and
Fig 3)
Janusz Ostrowski


PROFESSOR JOHN STEWART CAMERON, MD,
FRCP, CBE 1934-2023
Consultant Nephrologist (retired) Charing Cross Hospital, London
malcolm.phillips101@gmail.com
Dr Malcolm Phillips

Maria Kalientzidou
Katarina Derzsiova
Vincenzo Savica
Murat Aksu
Abdullah Yildiz
Mario Lamagna
Councillors:
Speakers:
Aciduman A
(Türkiye)
Aksu M
(Türkiye)
Ardaillou R
(France)
Balat Ayse
(Türkiye)
Bisaccia C
(Italy)
Credendino O
(Italy)
De Santo NG
(Italy)
De Santo MR
(Italy)
Derzsiovà K
(Slovakia)
Diamandopoulos A
(Greece)
Gembillo G
(Italy)
Gigliotti G
(Italy)
Kalientzidou M
(Greece)
Koulouridis Efstathios
(Greece)
Kurkus J
(Poland/Sweden)
Lamagna M
(Italy)
Mussi D
(Italy)
Ostrowski J
(Poland)
Philips M
(UK)
Rutkowski B
(Poland)
Savica V
(Italy)
Stefanidis I
(Greece)
Viggiano D
(Italy)
Widmer D
(USA)
Yildiz A
(Türkiye)
Faculty:
Bellinghieri G
(Italy)
Iorio L
(Italy)
Eknoyan G
(USA)
Calò L
(Italy)
Kazancioglu R
(Türkiye)
Ricciardi B
(Italy)
San Ayla
(Türkiye)
Smogorzewski M
(Poland/USA)
Mezzogiorno A
(Italy)
Scientific secretary:
for information email to
davide.viggiano@unicampania.it
Organizing secretariat:
Galileo Eventi - email:
galileoeventi@gmail.com
The program of the event will be posted on the IAHN website and the Galileo Eventi website:
https://www.iahn.info
https://www.galileoeventi.it
Davide Viggiano
Congress President

Professor Zbylut Twardowski
Professor
Zbylut
Twardowski
was
born
on
2
June
1934
in
Stanisławice,
Poland.
He
began
his
education
during
the
Second
World
War.
He
passed
his
secondary
school
leaving
examinations
with
honours
in
Chorzów
Batory
in
1952
and
in
the
same
year
commenced
medical
studies
at
the
Faculty
of
Medicine
of
the
Medical
Academy
in
Krakow,
which
he
completed
with
honours
in
January
1959.
In
July
1959,
he
started
working
at
the
Emergency
Station
in
Krakow
and
as
a
volunteer
assistant
at
the
2nd
Clinic
of
Internal
Medicine
at
the
Medical
Academy
in
Krakow,
where
he
took
part
in
the
organisation
of
the
Dialysis
Centre
of
the
Clinic.
In
1962,
he
was
employed
there
as
an
assistant.
In
1963,
he
moved
to
the
Mining
Hospital
in
Bytom,
where
within
a
year
he
organised
the
4th
Department
of
Internal
Medicine
including
the
Dialysis
Centre.
In
1963
he
obtained
his
first
degree
of
specialisation
in
internal
medicine.
In
1964
he
was
awarded
the
degree
of
Doctor
of
Medicine
on
the
basis
of
his
thesis
"On
the
advantages
and
possibility
of
constructing
an
artificial
capillary
kidney".
In
the
autumn
of
1966,
he
obtained
his
second
degree
of
specialisation
in
internal
medicine.
In
the
same
year
became
a
member
of
the
Transplantation
Commission
of
the
Ministry
of
Health
and
Welfare.
In
1968,
he
became
head
of
the
Department
of
Internal
Medicine
in
the
Mining Hospital in Bytom. In 1969 spent 3 weeks in the UK, where he
visited
several
nephrology
centres.
In
1972
he
did
a
month's
internship
at
the
Medical
Renal
Unit,
Royal
Infirmary,
University
of
Edinburgh,
Scotland.
In
1974,
he
visited
several
dialysis
centres
in
northern
Italy,
including
Bologna,
Padua
and Milan.
In
1975,
he
successfully
defended
his
habilitation
thesis
entitled:
"On
the
adequacy
of
haemodialysis
in
the
treatment
of
chronic
renal.
failure".
From
September
1976
to
August
1977
he
worked
as
a
fellow
in
the
Division
of
Nephrology,
Department
of
Medicine,
University
of
Missouri,
Columbia,
Missouri.
In
September
1977,
he
moved
to
Lublin,
where
he
became
Head
of
the
Department
of
Nephrology,
Institute
of
Internal
Medicine,
Medical
Academy,
in
1978.
In
the
same
year,
he
became
a
member
of
the
Commission
for
the
Development
of
Dialysis
and
Transplantation
of
the
Ministry
of
Health and Welfare and the Nephrology Commission of the Polish Academy of Sciences
In
July
1981,
he
again
left
for
the
United
States
and
took
up
a
post
as
Research
Fellow
at
the
Division
of
Nephrology,
Department
of
Medicine,
University
of
Missouri,
Columbia,
Missouri.
Here,
the
Professor
was
found
by
the
martial
law
introduced
in
Poland.
In
1982,
he
was
employed
as
Visiting
Associate
Professor
at
the
Department
of
Medicine,
University
of
Missouri.
In
1985,
he
was
promoted
to
Professor
in
the
Department
of
Medicine
of
this
University
and
Director
of
the
Peritoneal
Dialysis
Clinic
in
the
Division
of
Nephrology.
From
1983,
he
took
up
the
position
of
Staff
Physician
in
Nephrology,
Harry
S.
Truman
Memorial
Veterans
Hospital,
Columbia,
Missouri.
In
1987,
he
was
promoted
to
a
permanent
professorship
(Professor
with
tenure
in
the
Department
of
Medicine,
University
of
Missouri).
From
1991
-1999,
he
worked
as
an
Investigator
at
the
Dalton
Research
Center,
University
of
Missouri,
Columbia,
Missouri.
He
retired
in
1999
and
received
the
privileges
of
Professor
Emeritus
of
Medicine
at
the
same
University.
He
has
worked
closely
with
great
figures
in
nephrology, including Karl Nolph and others.
Professor
Twardowski's
main
clinical
interests
and
achievements,
carried
out
initially
in
Poland
and
later
in
the
United
States,
were
connected
with
renal
replacement
therapy,
particularly
peritoneal
dialysis
and
haemodialysis.
At
the
beginning
of
his
career,
he
was
also
interested
in
problems
of
kidney
transplantation,
including
those
from
living
donors.
As
early
as
1964,
he
patented
a
capillary
dialyser
in
Poland,
and
in
1965
an
improved
version.
This
was
the
first
patent
in
the
world
in
this
field.
Unfortunately,
it
was
not
possible
to
manufacture
such
a
dialyser
in
Poland,
but
this
was
done
somewhat
later
by
American
constructors.
This
type
of
dialyser
is
now
in
widespread
used
throughout
the
world.
Further
patents
related
to
swan
neck
catheters
for
peritoneal
dialysis,
presternal
catheters
for
peritoneal
dialysis,
new
types
of
haemodialysis
catheters
resistant
to
clot
formation,
as
well
as
machines
for
daily
home
haemodialysis.
In
total,
he
has
patented
23
solutions
for
renal
replacement
therapy
in
Poland,
the
United
States
and
other
countries
around
the
world,
including all European countries.
He
was
also
involved
in
describing
a
new
method
of
peritoneal
dialysis,
the
continuous
ambulatory
peritoneal
dialysis
(CAPD),
the
peritoneal
equilibration
test
(PET),
which
is
still
used
in
every
peritoneal
dialysis
centre
in
the
world,
was
one
of
the
first
to
propose
more
frequent
and
longer
haemodialysis,
and
a
specific
type
of
arteriovenous
fistula
puncture
called
butonholes.
He
was
also
the
author
of
180
abstracts,
nearly
400
articles
and
book
chapters,
7
teaching
videos,
and
24
letters
to
editors.
He
presented
500
lectures
at
scientific
conferences
and
was
chairman
of
approximately
100 scientific sessions.
Professor
Zbylut
Twardowski
was
a
member
of
many
scientific
societies
around
the
world.
These
included,
in
particular,
membership
of
the
Polish
Medical
Association,
Polish
Society
of
Internal
Medicine,
European
Renal
Association-European
Dialysis
and
Transplant
Association,
International
Society
of
Nephrology,
Polish
Society
of
Nephrology
(honorary
member),
American
Medical
Association,
American
College
of
Physicians,
American
Society
of
Artificial
Internal
Organs,
Member,
International
Society
for
Peritoneal
Dialysis,
American
Society
of
Nephrology,
Colombian
Society
of
Nephrology
(honorary
member),
International
Society
for
Hemodialysis
and
International
Society
for
Hemodialysis.
He
was
also
founding
editor
of
Hemodialysis
International,
editor
–
in
–
Chief
of
Hemodialysis
International,
Associate
Editor
Peritoneal
Dialysis
International,
Associate
Editor
of
Advances
in
Peritoneal
Dialysis,
Editor
of
Hemodialysis Today, and also Associate Editor Peritoneal Dialysis Today in the years 1985 - 2001.
He
received
numerous
awards
and
honours
for
his
exceptionally
active
work
and
scientific
achievements.
These
include
the
American
Kidney
Fund
Torchbearer
Award,
Best
Doctors
in
America,
Who's
Who
in
the
World,
silver
medal
of
the
Polish
Society
of
Pediatric
Nephrology,
Medicus
sapiens
renes
sani
liberi
ridentes",
International
Society
for
Haemodialysis
Belding
H.
Scribner
Trailblazer
Award,
2004
Lifetime
Achievement
Award
of
the
National
Kidney
Foundation, honorary membership of the Polish Society of Nephrology (2009) and many others.
Professor
Zbylut
Twardowski
achieved
his
first
greatest
successes
in
Poland
during
a
very
difficult
economic
and
political
situation,
before
the
‘Iron
Curtain’
was
broken
down
and
later
on
also
in
the
United
States,
where
he
continued
his
extremely
fruitful
clinical
and
scientific
career.
This
was
characterised
by
a
drive
to
discover
new
possibilities
in
renal
replacement
therapy
and
to
improve
these
pursuits.
All
his
activities
were
directed
towards
improving
the
effectiveness
of
treatment
and
the
welfare
of
patients
with
chronic
kidney
disease.
Many
of
his
insights
and
predictions
are
still
relevant
today
around
the
world,
including
Europe,
therefore
Professor
Zbylut
Twardowski
can
be
considered
as
one
of
the
leaders
in
the
development
of
renal
replacement
therapy,
particularly
dialysis
therapy.
The
death
of
Professor
Zbylut
Twardowski
is a great loss to the entire nephrology community worldwide.
Andrzej Więcek (ERA Past-President)
Janusz Ostrowski (IAHN Past-President)
Photo Janusz Ostrowski, Exhibition ERA-EDTA Congress 2010
Janusz Ostrowski


PROFESSOR ZBYLUT JÓZEF TWARDOWSKI (1934-2024).
IN MEMORIAM.
1
Head of the Department of Nephrology, Transplantation
and Internal Medicine, Medical University of Silesia, Katowice, Poland
2
Professor, Department of the History of Medicine,
Centre of Postgraduate Medical Education, Warsaw, Poland
Andrzej Więcek
1
, Janusz Ostrowski
2

Luigi Iorio, Division of Nephrology, De Bosis Hospital, Cassino:
Conferences on Kidney Failure and Heart Failure
Nicola De Napoli, Teresa Papalia, Division of Nephrology, Annunziata Hospital Cosenza:
Telesio Conferences on Edema, Sister Program of the International Society of Nephrology
Guido Bellinghieri and Vincenzo Savica, Division of Nephrology University of Messina:
Taormina course,
Mediterranean Kidney Society, International Federation of Kidney Foundations
Natale Gaspare De Santo, Giovanbattista Capasso, Massimo Cirillo,
7th European Colloquium on Renal Physiology,
Borelli Conferences on Acid-Base Balance, Visiting Professor of the University Luigi Vanvitelli, Conferences
of the Italian Institute of Philosophical Studies on Human Clinical Research: Ethics and Economics (1997)
and Survival is Not Enough (2007-2020), Bulgarian Assocaition of Professors Emeriti (2020)
The
Balkan
Cities
Association
of
Nephrology,
Dialysis,
Transplantation
and
Artificial
Organs
(BANTAO)
Professor
Nenov
was
one
of
the
key
persons
that
made
possible
The
Balkan
Cities
Association
of
Nephrology,
Dialysis,
Transplantation
and
Artificial
Organs
(BANTAO).
BANTAO
(Figure2)
Connects
Nephrologists
from
the
Balkan
Cities
not
Balkan
Countries.
The
Balkan
Cities
Association
of
Nephrology,
Dialysis,
Transplantation
and
Artificial
Organs
(BANTAO)
was established in Ohrid, Republic of North Macedonia on October 9, 1993. (Figure 3)
Janusz Ostrowski


PROFESSOR DIMITAR NENOV (1933 – 2024).
THE FOUNDER OF THE BANTAO JOURNAL
Former Head of the Nephrological Laboratory IV
th
Internal Clinic
University Hospital of L. Pasteur, Košice, Slovak Republic
Dipl. Ing. Katarina Derzsiova

Professor
Dimitar
Nenov
retired
in
2001
after
a
prolific
44-year
career.
His
scientific
and
organisational
activities
did
not
cease.
During
the
following
years
of
his
life,
he
continued
to
organise
annual
educational
courses
-
seminars
in
nephrology
under
the
title,
"Hot
Topics
in
Nephrology"
with
the
participation
of
leading
national
and
international
experts.
He
also
set
up
a
small
private
holiday
haemodialysis
centre
which
operated
every
summer
and
provided
regular
dialysis
treatment
to
dialysis
patients,
especially
those
from
abroad.
This
enabled
them
to
holiday
in
nearby
seaside
resorts
during
the
summer
holidays (12). This opportunity was also offered to our dialysis patients.
As
a
member
of
the
editorial
board
of
the
BANTAO
Journal
and
a
member
of
the
International
Federation
of
Kidney
Foundations,
he
became
Professor
Emeritus.
Later,
Professor
Nenov,
together
with
ten
other
professors
representing
five
universities in Varna, was the founder of the Bulgarian Association of Emeritus Professors and was elected its President.
Professor
Dimitar
Nenov,
always
smiling,
good-tempered,
very
friendly,
and
pleasantly
talkative,
will
be
missed
not
only
by
Bulgarian
nephrologists,
nephrologists
of
the
whole
Balkan
Peninsula,
but
also
by
many
nephrologists
from
all
over the world and, finally, by myself.
(Fig 4.)
.
His life's journey is over, our friend Dimitar left.
Honor to his memory.
Katarina Derzsiova
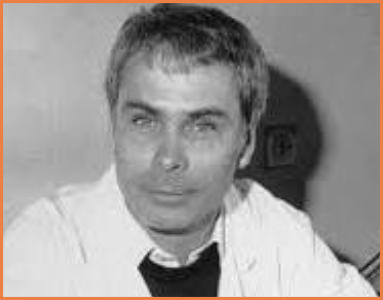
Stewart Cameron
Stewart Cameron
Stewart the Clinician
John Feehally: Stewart the Nephrologist
John
recalled
how
Stewart,
as
Professor,
built
up
the
Renal
Department
from
when
appointed
Professor.
From
the
start
he
promoted
the
concept
of
a
“renal
family”,
incorporating
all
staff
involved
in
the
care
of
renal
patients,
and,
most
importantly,
the
patients
themselves.
He
devoted
himself
to
clinical
and
scientific
nephrology.
Dialysis
of
patients
with
chronic
renal
failure
(CRF)
was
started
and
he
recognised
the
need
for
an
active
renal
transplant
programme.
Care
of
children with renal diseases was commenced.
He
had
earlier
spent
a
year
at
Cornell
University
(1962-63)
researching
proteinuria/selectivity,
and
there
first
encountered
dialysis
and
transplantation
for
End-Stage
Renal
Failure
(ESRF).
His
interest
in
glomerular
diseases
led
to
his
becoming
a
leading
authority
on
glomerulonephritis
(GN).
John
referred
to
Stewart’s
wide-ranging
contributions
to
nephrology,
including
paediatric
nephrology,
lupus,
urate
metabolism
and
the
history
of
nephrology.
He
trained
over
250
juniors
and
fellows from all over the world; many became senior figures in the specialty and other areas of medicine.
Chisholm Ogg: Working with Stewart
It
was
a
delight
to
listen
to
Stewart’s
closest-working
colleague
for
nearly
30
years
and
a
friendship
extending
over
50
years.
Chisholm
was
instrumental,
with
Stewart,
in
developing
the
Guy’s
renal
centre
including
paediatric
nephrology.
He
recounted
weekly
meetings
with
other
specialties:
radiology,
nuclear
medicine,
pathology
and
paediatrics-all
examples
of
the “renal family” concept which permeated the service and contributed so much to its success and fame.
Chisholm
amusingly
described
the
initial,
limited
dialysis
facilities
followed
by
the
subsequent
expansion
involving
adult
and child dialysis and the start. of transplantation.
Diana Sale, Penny Powis: Stewart and the Renal Family
The
meeting
would
have
been
incomplete
without
hearing
from
senior
nursing
staff
who
worked
on
the
renal
unit.
The
theme
of
the
renal
family
came
across
strongly,
both
clinically
and
personally.
It
was
clear
from
both
that
nurses
“ran
the
dialysis
unit”,
carrying
out
what
were,
at
that
time,
considered
non-nursing
procedures
(as
well
as
social
activities!).
Such
actions
were
frowned
upon
by
the
Guy’s
nursing
hierarchy!
But
importantly,
“everyone’s
opinion
was
valued”
and
“patients were partners in their care”.
Through the nursing team the first nurse-training course in dialysis in the UK was created.
Geoff Koffman: Stewart and Kidney Transplantation
Geoff
gave
an
illuminating
review
of
transplantation
at
Guy’s
in
which
he
had
played
a
significant
role
as
transplant
surgeon.
Transplantation
started
in
1966.
In
the
first
5
years
about
200
operations
were
performed.
In
1968
the
first
transplant of a child occurred leading to the establishment of the first children’s dialysis and transplant unit in the UK.
Transplantation
grew
rapidly.
There
are
now
11
transplant
surgeons
at
Guy’s
carrying
out
approximately
300
transplants
/year.
Live
donor
transplantation
was
promoted,
increasing
from
5-10
per
annum
to
over
100.
In
1995
a
kidney-pancreas
transplant
programme
for
diabetics
was
successfully
introduced.
Stewart’s
role
in
transplantation
was
prominent,
particularly promoting low-dose steroids and transplantation of elderly patients with ESRF.
Cyril Chantler: Stewart and Paediatric Nephrology
Stewart
was
significantly
involved
in
the
early
phase
of
paediatric
nephrology,
introducing
it
soon
after
he
became
Professor.
By
1970,
11
children
had
been
treated
by
dialysis
/transplantation.
Stewart
wrote
his
first
paediatric
paper
in
1971.
His
role
in
this
area
led
to
him
being
made
President
of
the
European
Society
of
Paediatric
Nephrology
(1975).
Both
Cyril
and
Stewart
focused
closely
on
adolescents,
emphasising
the
need
for
attention
to
treatment
at
this
stage
in
a
child’s
development.
I
cannot
but
include
some
amusing
stories
involving
Stewart.
Cyril
recalled
a
conversation
with
an
eminent,
older
consultant
who
stated
how
lucky
it
was
to
have
Stewart
on
the
staff
and
how
intelligent
he
was.
Cyril
concurred.
“It’s
just
a
pity
he
doesn’t
wear
the
uniform”
was
the
next
comment!
Stewart’s
dress
code
was
often
referred
to
during
the
Celebration Day with affection and laughter.
Stewart the Investigator
Richard Glassock: Stewart and Glomerular Disease-the Early Years
Richard,
appearing
by
video-link
from
California
referred
to
Stewart’s
first
papers:
in
J.
Clin
Invest
(1964)
-
proteinuria
in
the
nephrotic
syndrome
(NS),
Lancet
(1965)
-
proteinuria
in
children
with
NS
and
the
BMJ
(1966)
-
treatment
of
proliferative
nephritis
and
NS.
Other
papers
followed
in
the
BMJ
signalling
that
Stewart
was
in
the
forefront
of
work
in
glomerular
disease.
Richard
followed
Stewart’s
career
with
great
interest
and
in
1988
they
jointly
wrote
a
book
on
NS
which
is
still
quoted today.
Richard
and
Stewart
were
firm
friends.
We
will
remember
Richard’s
parting
words
in
his
talk,
translated
from
Gaelic:“Farewell my friend, until we meet again”.
Andy Rees: Stewart and Glomerular Disease-After That
Andy
recounted
his
first
“out-of-the-blue”
meeting
with
Stewart
which
occurred
with
less
than
24
hours’
notice
from
Andy.
He
was
appointed
at
Guy’s
a
few
months
later,
though
he
did
not
attribute
that
to
Stewart’s
influence
but
partly
because he was wearing his only suit!
Andy
regarded
Stewart
as
being
responsible
for
nephrology
“moving
on”
from
primitive
descriptions
of
GN
such
as
“Ellis
types
I
and
II”,
and
minimal-change
GN
(MCGN)
being
early
membranous
GN
having
a
50%
mortality
without
steroid
treatment.
Stewart
reclassified
GN
initially
with
data
on
MCGN,
membranous
GN
and
proliferative
GN
in
adults
and
children. Later classifications by Stewart were even more detailed.
Stewart
was
the
first
to
use
Venn
diagrams
in
nephrology
and
introduced
actuarial
survival
curves
in
various
forms
of
GN,
-work
of
international
renown.
He
showed
that
survival
in
NS
was
directly
related
to
the
degree
of
proteinuria
-a
finding
confirmed
ever
since.
He
published
studies
on
complement,
platelet
activation
and
glomerular
macrophages
and
T-cell
substrates in GN. Much of this data lead to the testing of new therapies.
Liz Lightstone: Stewart and Lupus
Liz
started
her
talk
(by
video)
indicating
that
Stewart
published
extensively
on
lupus
nephritis
(LN).
He
had
stressed
the
importance
of
using
low-dose
steroids
in
lupus
because
of
the
morbidity
and
mortality
associated
with
high-doses.
His
work
also
showed
the
necessity
of
long-term
follow-up
of
patients,
the
importance
of
lupus
in
relation
to
pregnancy
and
the need for randomised controlled trials in its treatment.
In
a
Lancet
paper
(1970)
he
wrote
on
the
steroid-saving
effect
of
cyclophosphamide
in
LN.
He
challenged
the
view
that
LN
was
a
benign
disorder
pointing
out
the
published
high
mortality
rates.
But
in
1999
he
reported
long-term
results
in
116
patients
treated
at
Guy’s
with
low-dose
steroids
and
azathioprine,
showing
improved
survival.
Stewart
also
published
significant data on childhood lupus.
Stewart the Influencer
Chris Winearls: Stewart the UK Leader
Chris
described
organisational
events
occurring
before
the
International
Society
of
Nephrology
(ISN)
congress
in
1993
with
Stewart
as
President.
Chris
was
a
secretarial
helper,
or,
as
he
put
it,
“a
bag-carrier”!
Stewart
overcame
major
these
problems
with
great
expertise.
The
meeting
was
a
success
and
significantly
enhanced
the
standing
of
UK
nephrology
in
the eyes of the wider world.
As
President
of
the
UK
Renal
Association
(1992-1995)
Stewart
fought
for
greater
funding
for
renal
services.
The
recognition
of
his
major
position
in
nephrology
contributed
to
success.
By
retirement
he
had
“made
UK
nephrology
respectable”
as
well as being recognised as a world-leader in the specialty.
Pierre Ronco-Stewart in European Nephrology
In his absence John Feehally presented using Pierre’s slides.
Pierre
noted
that
Stewart
was
a
delegate
at
the
founding
meeting
of
the
ERA-EDTA
(1964).
He
was
editor
of
the
Proceedings
of
its
congresses
1970-1973.
From
1984-1987
he
was
President
and
in
1985
was
involved
in
creating
“Nephrology, Dialysis and Transplantation”; he was a member of the journal’s Editorial Board 1986-1993.
One
of
Pierre’s
slides
struck
home.
He
quoted
Stewart
stating
that
both
the
science
and
the
clinical
practice
of
nephrology
were
vital.
In
a
cautionary
frame
of
mind,
Stewart
added
“There
are
good
scientists
among
young
doctors,
but
are they shaking the hands of patients at midnight?”-A message for Europe and beyond.
Jo Adu: Stewart and the Development of Global Nephrology
Jo
began
(by
video)
describing
the
Guy’s
unit
as
a
“United
Nations
of
doctors
and
scientists”
referring
to
the
number
and
range
of
nationalities
in
the
team.
He
described
changes
within
the
ISN
to
spread
its
messages
to
the
developing
world.
As
President
of
the
ISN,
Stewart
was
committed
to
global
development
and
the
Committee
for
the
Global
Advancement
of
Nephrology
was
established
subsequently.
This
led
to
developments
such
as
the
Fellowship
Training
Programme
and
the
Sister
Renal
Center
Programme,
among
others.
From
2001
nephrology
flowered
in
Africa,
the
Middle
East
and
Asia.
Now, the ISN features in 153 countries and has over 9000 members.
Stewart’s view that ISN should spread nephrology world-wide is now a reality.
Leon Fine: Stewart the Writer and Historian
It
is
pertinent
to
report
here
that
Leon
(by
video
from
US)
described
Stewart
as
“the
most
prominent
member
of
the
IAHN”,
and
“he
was
the
history
of
nephrology”
writing
over
50
papers
on
this
topic.
He
helped
establish
a
series
of
in-
depth,
recorded
interviews
with
prominent,
but
retired,
nephrologists
which
led
to
the
formation
of
this
Association.
In
2013 his contributions in this field were recognised with Honorary Membership of IAHN.
Ian Abbs: Stewart’s Impact through Guy’s
High
praise
when
Ian
stated
that
Stewart
“with
others,
paved
the
path
for
the
future
of
Guy’s”.
The
multi-professional
team
model
contributed
to
this.
He
helped
to
change
a
rigid
hierarchical
period
in
which
creativity
was
frowned
on
to
the
“foundational”
period
of
the
70’s.
The
multi-disciplinary
team
approach
was
more-or-less
an
innovation
in
British
medicine. Patient’s needs were put first.
Here
I
digress
again
into
an
amusing
story
from
Ian’s
personal
experience.
On
a
ward
round
Ian
presented
the
case
of
a
lady
with
interstitial
nephritis
the
cause
of
which
had
eluded
him.
He
felt
that
Stewart
was
not
listening.
But
Stewart
picked
up
the
patient’s
handbag
and
started
rummaging
through
it!
After
a
while
Stewart
held
up
some
pills-the
patient
called them her “little helpers”. “Are they by any chance called Naproxen?” Stewart asked. They were! Aetiology solved!
Where are We Now?
Sharlene Greenwood: Multi-Professional Care in 2004
Sharlene,
Renal
Physiotherapist-
a
profession
not
heard
of
by
many
in
the
audience,
but
clearly
another
branch
of
the
“renal family”.
Sharlene
stressed
the
need
for
clinicians
to
address
all
of
a
patient’s
needs.
She
described
the
establishment
of
the
Renal
Services
Transformation
Programme-
a
multi-professional
workforce
formed
in2020,
including
counsellors,
physiotherapists, occupational therapists and renal psychologists. Recruitment to these positions is occurring gradually.
Sharlene recognised the early contribution to this concept made by Stewart and his team.
Neil Turner: Nephrology in 2024
Neil
showed
data
from
the
1960’s
to
recently
on
the
global
numbers
of
patients
on
dialysis
and
those
with
functioning
transplants.
Whilst
numbers
of
dialysis
patients
have
more-or-less
plateaued,
transplant
numbers
have
risen
substantially
and continue to do so.
In
terms
of
current
focus
on
renal
diseases
Neil
outlined
work
in
1979
on
2500
patients
with
glomerular
disease,
including
data
from
Guy’s,
on
the
relationship
of
the
degree
of
proteinuria
in
relation
to
kidney
survival.
This
year
a
paper
with
data
on
over
12,000
patients
from
renal
registries
world-wide
showed
that
glomerular
disease
is
still
a
major
cause
of
loss
of
kidney
function
and
that
the
degree
of
proteinuria
still
relates
to
survival
of
kidney
function.
Treatment
with
ACE
inhibitors,
Angiotensin
II
receptor
antagonists
and
more
recently
aldosterone
antagonists
may
be
beneficial
to
many
patients otherwise heading towards ESRF.
Ian Abbs, Cyril Chantler, John Feehally: Summing Up
Between
them,
tribute
was
paid
to
the
support
received
from
Guy’s,
Kings
and
the
UK
Kidney
Association
and
particularly
to John for his planning and organisational work, in making this Celebration of Stewart’s life and achievements possible.
It
had
been
a
truly
inspirational,
happy
and
fitting
event,
ending
with
old
friends
being
invited
to
meet
in
the
bar
in
true
“Stewart style”.
I
can
do
no
better
than
to
end
with
a
quotation
from
Stewart
himself:
“Friendship
should
remain
as
a
primary
value,
as
friendship is important in every human endeavour”
INFO FROM POLAND
As
in
previous
issues
of
the
IAHN
Bulletin,
I
am
providing
a
brief
update
on
the
most
important
nephrology
events
that
took
place
in
Poland
in
the
first
half
of
2024.
The
first
of
these
was
the
Gdańsk
Nephrology
Review
POST
ASN
Meeting,
which
has
been
held
for
20
years.
It
took
place
on
January
12-13.
Janusz
Ostrowski
delivered
a
lecture
titled
"The
History
of
Urine Examination" (Figures 1, 2).
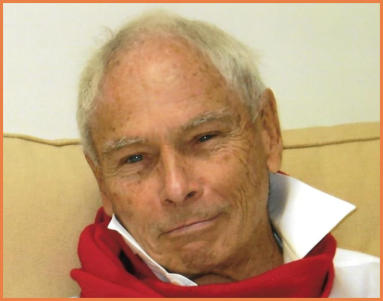
Announcement:
XIII IAHN Meeting, Naples
Dear Distinguished Colleagues,
We
are
pleased
to
inform
you
that
the
XIII
Congress
of
the
International
Association
for
the
History
of
Nephrology
(IAHN)
will be held in Naples, Italy.
To
ensure
a
smooth
event
experience,
the
meeting
dates
have
been
shifted
to
Friday,
November
15th
-
Sunday,
November
17th, 2024.
This
marks
a
significant
homecoming
for
IAHN.
In
1993,
Italy
(Cassino)
hosted
the
inaugural
congress,
laying
the
foundation
for
a
vibrant
field.
Thirty
years
later,
a
wealth
of
data
has
been
collected,
with
over
500
original
manuscripts
published in international journals.
The
Congress
celebrates
the
remarkable
progress
of
nephrology,
in
the
boundary
zones
of
other
disciplines
and
its
entry
into
scientific
parlance
in
the
1950s
of
the
twentieth
century,
yet
with
roots
extending
well
beyond
the
work
of
Thomas
Addis. Fueled by advancements like dialysis, it has rapidly evolved to address the needs of millions worldwide.
The
2024
IAHN
meeting
delves
into
the
fascinating
history
of
kidney
disease
treatments,
offering
a
unique
perspective
on
the
latest
therapeutic
breakthroughs.
This
will
allow
us
to
better
understand
the
latest
therapeutical
advances
(such
as
HIF
inhibitors,
new
drugs
for
IgA,
MCO
filters,
glyflozins,
new
mineralocorticoid
antagonists,
new
CNI,
anti-Bliss,
etc.)
from
a
historical
perspective.
This
exploration
will
inspire
new
historical
inquiries
and
a
deeper
understanding
of
contemporary
treatments.
Join
us
in
celebrating
the
History
of
Nephrology
in
Italy.
Network
face-to-face
with
prestigious
Italian
and
international
researchers
in
the
field,
fostering
collaboration
and
sparking
new
research
ideas.
The
congress
will
feature
captivating
plenary lectures by prominent Italian and global experts, encouraging active participation from young scientists.
Don't miss this opportunity to connect, celebrate, and propel the future of nephrology history!
Venue: Camaldoli Hermitage, Naples. From the airport to the Hermitage, it takes less than 30 minutes by car or taxi.

Figure 1. Professor Boleslaw Rutkowski, main organizer
(photo Janusz Ostrowski)

Figure 2. Professor Janusz Ostrowski
(photo Maria Ostrowska)
Another
important
event
was
the
conference
related
to
the
World
Kidney
Day
traditionally
organised
by
Prof.
Ryszard
Gellert on March 15. Przemysław Rutkowski and Janusz Ostrowski also actively participated in this meeting (Figures 3, 4).

Figure 3. Professor Janusz Ostrowski

Figure 4. From left: Professors Przemysław Rutkowski,
Janusz Ostrowski, Ryszard Gellert
Next
was
the
Scientific
and
Training
Conference
"Nephrocardiology
2024"
held
on
April
19-20
in
Białystok,
where
Bolesław
Rutkowski and Janusz Ostrowski demonstrated their active participation (Figures 5, 6).

Figure 5. Professor Bolesław Rutkowski.
(photo. Janusz Ostrowski)

Figure 6. Professor Janusz Ostrowski. First right.
(photo. Maria Ostrowska)
On
May
8th,
I
participated
in
a
joint
scientific
session
organised
by
one
of
the
oldest
scientific
societies
in
Poland,
the
Krakow
Medical
Society,
together
with
the
Krakow
Society
of
Medical
History
Enthusiasts.
During
this
session,
I
presented
a lecture titled "Professor Zbylut Twardowski's Contribution to the Development of Nephrology" (Figures 7, 8).

Figure 7. Professor Janusz Ostrowski
(photo Maria Ostrowska)

Figure 8. From left: dr Adam Wiernikowski, prof. Władysław Sułowicz, dr Halina
Twardowska, prof. Janusz Ostrowski (photo Maria Ostrowska)

Figure 9. Professor Bolesław Rutkowski
(photo Janusz Ostrowski)

Figure 10. Professor Janusz Ostrowski, first left
(photo Leszek Domański)
OBITUARIES
Janusz Ostrowski


INFORMATION ABOUT NEXT IAHN CONGRESS
Department of Translational Medical Sciences,
Univ. of Campania “L. Vanvitelli”, Naples, Italy
Davide Viggiano

The
establishment
of
the
BANTAO
Journal
was
a
milestone
in
the
life
of
BANTAO,
which
was
launched
in
2003
in
Varna
at
the
6th
BANTAO
Congress.
The
BANTAO
Journal
represents
the
main
link,
the
glue
connecting
all
the
Association
members.
It
is
currently
published
twice
a
year.
Dimitar
Nenov
was
its
first
editor-in-chief
(2).
Professor
Mydlík
took
part
in
the
inaugural
ceremony
of
the
BANTAO
Journal,
which
has
made
its
mark
in
the
history
of
the
Balkan
Peninsula.
Professor
Mydlík
immediately
seized
the
opportunity
to
publish
in
this
incipient
journal.
Two
of
our
papers
presented
at
the
2003
BANTAO
Congress
were
published
in
the
same
year
(4,5).
The
number
of
our
publications
increased
thanks
to
the
consistent
assistance
of
the
journal
editors
(Momir
Polenaković,
Goce
Spasovski,
Ali
Basci,
and
others).
We
published
a
total
of
eight
papers
in
the
BANTAO
Journal
(4-11)
and
contributed
six
presentations
at
BANTAO
congresses
in
the
same
years.
Dimitar
Nenov
had
the
idea
of
establishing
a
National
Bulgarian
Nephrology
Journal,
which
would
be
free
of
language
barrier
for
Bulgarian
nephrologists.
He
implemented
his
idea,
founding
the
journal
Aktualna
Nefrologia
as
an
experiment
to
see
if
it
would
flourish
or
die
out.
The
journal
was
a
success
and
Nenov
was
not
just
the
founder
but
also
the
editor-in-
chief
of
the
journal.
In
1991,
at
his
initiative,
the
Varna
Kidney
Foundation
was
established.
In
addition,
he
was
a
founder
of
the International Federation of Kidney Foundations (IFKF).
Our
friendship
with
Professor
Nenov
has
been
a
tradition
since
the
last
decade
of
the
last
century.
We
met
most
often
in
Sicily
at
the
Nephrology
Courses
in
Taormina
,
organized
by
Professors
Guido
Bellinghieri
and
Vincenzo
Savica.
Professor
Nenov,
Professor
Mydlík
and
later
I,
were
regular
lecturers.
In
that
pleasant
environment
and
company,
our
friendship
was
strengthened
especially
thanks
to
the
opportunity
to
talk
in
the
common
Czech-Slovak
language.
Professor
Nenov
was
fluent
in
Czech.
He
learned
Czech
in
1966
during
a
stay
in
Prague
at
the
Institute
for
Blood
Circulation
Diseases,
which
at
that time was headed by Professor Jan Brod, the doyen of nephrology in Czechoslovakia.
In
2006,
Professor
Mydlík
invited
Dimitar
Nenov
to
Košice
to
the
7th
International
Nephrology
Symposium
"
Metabolic
Changes
in
Chronic
Renal
Failure
",
which
was
held
on
awarding
the
honorary
degree
of
"Doctor
Honoris
Causa"
to
Professor
Vittorio
Bonomini,
M.D.,
from
the
University
of
Bologna,
Italy.
The
ceremony
took
place
in
the
Historical
Auditorium
of
the
P.
J.
Šafárik
University
in
Košice,
at
Rector's
Office.
The
following
day,
the
Symposium
was
held
in
the
Historical
Hall
of
the
East
Slovak
Gallery,
where
Professor
Nenov
presented
his
scientific
work
on
the
topic,
"Hepatitis
C
in
Haemodialysis
Patients
".
Other
lectures
were
given
by
eminent
nephrologists
from
Slovakia
and
Europe,
three
of
them,
Professors Guido Bellinghieri, František Kokot, and Vittorio Bonomoni, were Doctor Honoris Causa of our University.
Professor
Nenov
also
took
part
in
the
social
programme
during
that
festive
event,
the
"
Chamber
Music
in
the
St.
Michael
Chapel",
the
"Sightseeing
Tour
in
the
Historical
Part
of
Košice”,
and
the
farewell
dinner
hosted
by
the
celebrant,
Professor
Bonomini,
and
his
son.
At
the
end
of
his
stay,
Dimitar
Nenov
visited
"Nephron"
,
our
private
Dialysis
Centre
in
Košice (Fig. 3.).
I
had
met
him
together
in
the
90s
through
mutual
friends
Vincenzo
Savica,
Natale
De
Santo
and
Shaul
Massry
during
a
scientific meeting in Varna and an affectionate friendship was immediately born.
Dimitar
was
a
special
person,
he
was
a
great
gentleman,
he
had
the
character
traits
typical
of
a
Bulgar
man,
very
reserved, generous, sincere and above all very dignified with a keen intelligence.
Thanks
to
the
friendship
that
was
immediately
established,
I
had,
at
his
invitation,
the
opportunity
to
visit
Bulgaria
and
in
particular
the
beautiful
city
of
Varna.
during
the
annual
scientific
meetings
organized
by
him
on
behalf
of
the
Bulgarian
Kidney Foundation entitled "Hot topics in Nephrology".
By
virtue
of
his
interest
in
Sicily,
I
had
the
opportunity
to
invite
him
to
participate
in
the
international
nephrological
scientific
meetings
in
Taormina,
conferences
which
saw
his
active
participation
with
a
lecture
in
1998
during
the
V
Taormina (Fig. 1)
Janusz Ostrowski


DIMITAR NENOV IN SICILY (1998-2009)
President of the Italian Branch of European Association of Professors Emeriti,
National Councilor of Italian Association of Organs Tissues and Cells Donors,
Founder of the Mediterranean Kidney Society
Email: gbellinghieri@hotmail.com
Guido Bellinghieri


Proceedings of 5
th
Toarmina Course
on Nephrology 1998
Course
on
Nephrology
entitled
"Familial
Hyperlipidemia
Treatment
with
Monoclonal
LDL-Apheresis"
(1).
Also
interesting
was
the
lecture
on
"Fluid
and
electrolyte
balance
in
the
elderly"
which
he
then
gave
in
2000
(Fig.
2,
3)
during
the
VI
Taormina Course on Nephrology (2).

VI Taormina course on Nephrology 22 October 2000
He
also
took
an
active
part
in
Taormina
during
the
3rd
congress
of
the
International
Association
for
the
History
of
Nephrology
(IAHN)
in
November
2001
(Fig.
4.).
In
that
occasion
he
delivere
a
lecture
on
“Balkan
Nephropathy
A
Disorder
of
Renal Embryogenesis ? “ (3).
3
rd
congress of the International
Association for the History
of Nephrology Taormina 2001
His other interesting interventions saw him involved both during the VII Congress of the International
F
e
d
e
r
a
t
i
o
n
s
…
o
f
Kidney
Foundation
(IFKF)
in
2006
in
Giardini
Naxos
and
during
the
I
congress
of
the
Mediterranean
Kidney
Society
(MKS)
held in October 2009 in Taormina (Fig. 5, 6).

I
st
Mediterranean Kidney Society Congress Taormina
October 2009

I
st
Mediterranean Kidney Society Congress Taormina
October 2009
6
th
Taormina Course on Nephrology
2000
His
active
participation
in
the
aforementioned
scientific
meetings
was
always
punctual
and
precise
and
derived
from
his
vast scientific and healthcare knowledge in the nephrology field.
His
passing
will
deprive
us
of
his
smile,
his
elegance
in
presenting
himself
and
the
human
warmth
he
was
able
to
convey
to
those
who
were
lucky
enough
to
enjoy
his
friendship.
For
these
reasons,
dear
Dimitar,
you
will
always
remain
present
in
our memory.
References:
1.
Nenov
D,
Stoyanov
A,
Tchankova
P.,
Konovalov
G.:
Familial
Hyperlipidemia
with
Monoclonal
LDL-Apheresis.
Proceedings
of 5th Taormina Course on Nephrology. Ed. Bios 1998: 275-279.
2.
Todorova
V.S.,
Nenov
V.
D.,
Nenov
D.
S.:
Fluid
and
Electrolyte
Balance
in
the
Elderly
Proceedings
of
6th
Taormina
Course
on Nephrology. Ed. Bios 2000.: 99-105.
3. Nenov V. D., . Nenov D. S: “Balkan Nephropathy. A Disorder of Renal Embryogenesis? Am. J. Nephrol. 2002; 22: 260-265.